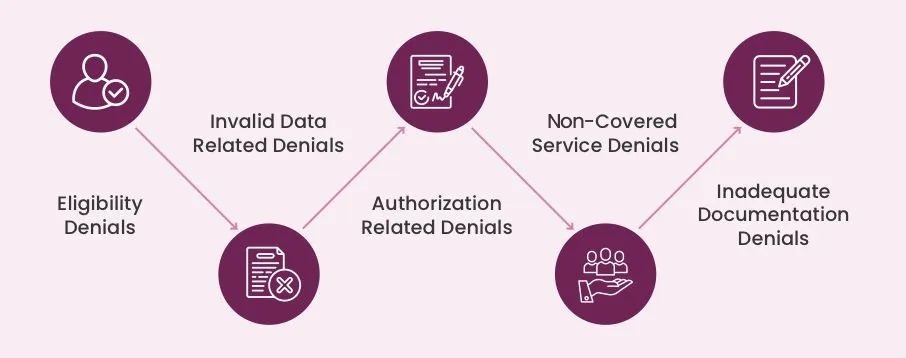
Do you know Why it happens?
Denials can happen for various reasons but are most often the result of an incorrect bill
or claim. When a health insurance company denies a claim, it can leave the provider
responsible for the full cost of the services provided. Enforcement usually occurs because
an insurer wants to return some of the money paid to the provider. Payment may have
been made through a healthcare financial intermediary, such as an insurance company
or Medicare.
A bill may also be denied if the professionals providing solutions are not medically
appropriate. Denial management services in medical billing extend beyond medical care
services. Denial of a health insurance claim can include insurance providers that won’t
pay for things like devices, diagnostic tests, services that are not covered by the
insurance, products that are not covered by the insurance, screening at a medical facility,
or if the provider who receives the bill is not licensed, that isn’t licensed by a licensed
entity.